7 rules for team communication
To have a successful team, communication is key. Here's how to communicate more effectively.
Despite the digitization of healthcare, most providers have yet to adopt communication strategies that correspond to modern expectations.

Streamlining communication and coordination was recently nominated as one of the top three trends in healthcare that will continue to influence investments and decision-making in 2022. Furthermore, the CMS has adopted a new Quality Strategy's Goal to promote effective communication and coordination of care.
Healthcare is an interdisciplinary field with many stakeholders. The coordination of care around a patient is a complex task that requires not only hands-on-management, but in particular seamless and effective communication with employees and colleagues across organizations, patients and their families. Especially in home health care, there is a constant need to communicate around patients and admin. Information may not always be as urgent compared to clinical settings, but it is equally important due to the high frequency of repetitive tasks and the relentless need to coordinate across time and space.
Poor communication costs a lot of time and money. Even worse, it leaves staff strained and unhappy, increasing turnover, and clients unsatisfied with the service they receive. In summary, efficient communication is critical for the success of every home care provider.
This article shows you the problem and offers the solution.
Most providers still depend on phone calls, emails, paper and faxes. However, we are beginning to understand that these one-way means of communication are ineffective and inefficient, resulting in errors, frustration, delays and bottlenecks.
Due to the large coverage areas of providers and the dynamic nature of home care, it is a big challenge to keep all staff informed. This includes communication between the office and the field as well as in the field between nursing and home care staff. In addition, the same information often has to be shared with different people, with emails, team meetings and paper being put to use haphazardly.
The phone is very popular - a leader in “synchronous communication” tools. This real-time exchange of information can be very time-consuming and stressful, especially for mobile workforces. When out and about, availability can be bad and numerous attempts have to be made to reach someone. The caller may have to leave voicemails without knowing if the message will reach the person on time. In addition, information cannot be traced backed or looked up at a later point in time, increasing errors and stress amongst staff. Calling is justified in some cases, during emergencies or to share urgent information quickly, but the cost for communicating non-urgent information on a daily basis is simply too high.
Emails, in contrast, rank high when it comes to “asynchronous communication” tools. Using emails confronts users with a different set of problems: information is isolated, group communication is chaotic and specific information can be very hard to find. People have to go through long email chains to gather relevant information. When someone replies to an email chain, all recipients are addressed, even if it is not relevant for them, or worse, relevant addressees are left out. Moreover, urgent information often arrives too late via email, or is drowned out by the noise of a full inbox.
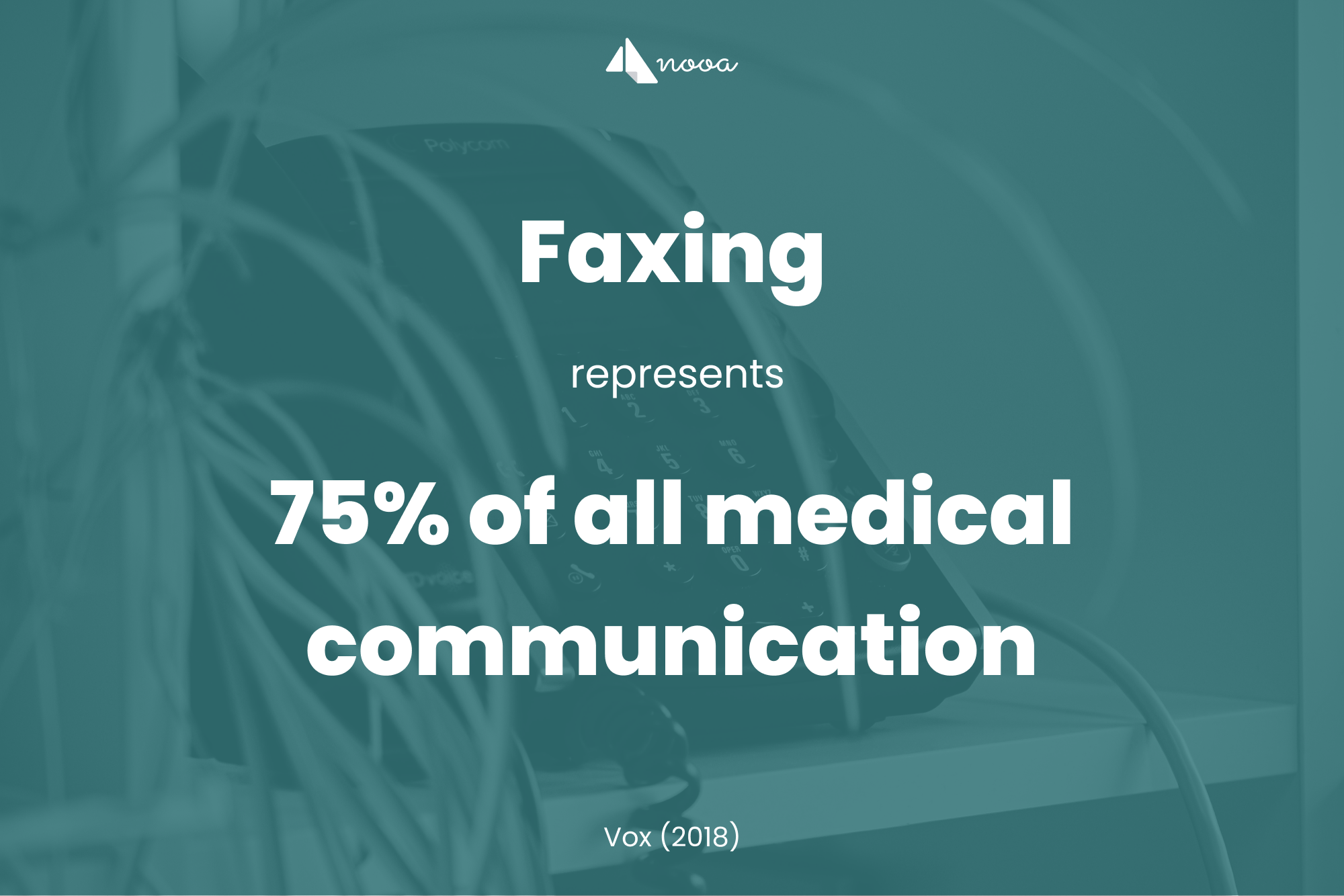
Faxes are often used to transmit patient data between providers and are another classic asynchronous communication tool. Unfortunately, faxes are still very popular and remain the de facto golden standard when it comes to medical communication, with studies showing that faxing represents 75% of all medical communication. While faxes do their job of transmitting files properly, they are not suited for sharing time-sensitive information nor for communicating with more than one recipient. Finally, they are certainly not suited for a mobile workforce which is out and about with clients, without a fax machine in sight.
To summarize: neither phone, emails nor faxes are suited to help health care providers share information in a way which helps them do their job efficiently. The aforementioned tools serve a specific purpose and are only effective in niche situations - however, unable to share information quickly and reliably with staff and clients, they are limited, outdated and not flexible enough to fit the needs of home care.
In order to overcome the limitations of phone, email and fax, organizations often introduce a messenger.
As of October 2021, two billion users were accessing WhatsApp on a monthly basis, making it by far the most popular mobile messenger application. Although an asynchronous tool like email and fax, most users perceive and use WhatsApp as a synchronous communication tool. In health care, physicians frequently use WhatsApp to communicate with peers and the clinical utility of this communication tool is on the rise, especially in acute settings. However, with WhatsApp, healthcare workers face two major problems.
The first problem is that WhatsApp does not comply with HIPAA regulations. Given the non-compliance with HIPAA, using it puts healthcare workers at risk to make errors when managing patient data. The safety of sensitive data cannot be guaranteed since it is stored locally on the device where it is used and there is no central access control and management. This makes it impossible to centrally recover and delete data.
Another issue is that the option to delete messages prevents effective auditing. Worse still, WhatsApp accounts are often used for private and work-related communication, exacerbating compliance issues. Healthcare organizations often try to circumvent these problems by introducing workarounds, for example obfuscating, abbreviating or codifying data to avoid unique identification of patients. While this usually creates confusion and misunderstanding, it does not solve the issue: having to share images, with which accompanying metadata such as date, time or geographical coordinates is transmitted, again leads to compliance issues that are not solved with workarounds.
Besides WhatsApp, many other messaging applications exist. Some of them face the same issues, lacking HIPAA compliance, while others comply with regulations. But why have these not been adopted in healthcare settings?
Here, we encounter the second problem: messengers are not suited for communication in healthcare. One of the issues users face with messengers concerns group chats. Since these are usually unstructured and undisciplined, individuals have a hard time following-up on information they require, since the stream of conversation has left them behind. In addition, they are cluttered with things that do not concern them, resulting either in information overload or in leaving the group. In both situations, recipients do not get the information they need, when they need it.
Since information in healthcare can be a matter of life and death, it needs to be both structured and targeted - a requirement that conventional messengers do not meet. In addition, most messengers are not portable and can only be used on one device. This is often further limited to use on a single mobile device, without access from a PC or tablet, making it impossible for care workers to work from multiple bases and locations. To summarize, even secure messengers do not meet the requirements of care communication to an extent where the costs justify the benefits.
So what about EMRs and care software? Good question. Some EMRs and care software have one or multiple communication features integrated somewhere in their systems. While these systems are adapted to healthcare needs, communication is not their primary use case. Compared to phone calls, emails, faxes and messaging, users are unable to communicate with EMRs and care software in the same way. This paradigm shift forces everyone to learn new ways of sharing information, making them a lot less efficient. To make matters worse, most communication features in EMRs and care software are very limited, usually reduced to basic one-to-one text messages, making group communication and media sharing impossible.
Furthermore, these systems are siloed and cannot properly connect staff to the people they need to be connected to, for example physicians or therapists, which use systems of their own. This leaves healthcare providers with disjointed systems, forced to bridge the information gap with phone, fax & co. Common shortcomings are:
In addition, EHR and care software-based messaging can be cumbersome, consuming a large part of the IT budget and failing to scale across the organization. Software providers often struggle to support urgent and emergent communication, and most do not offer the feature-rich communication tools that care teams need to collaborate effectively.
Given the shortcomings of EHRs and care software when it comes to communication, many providers still use unsafe messengers or outdated technology to share information with their teams or with other healthcare providers.
From the myriad of tools that we have discussed, not one of them meets the requirements that home health providers need. As a result, providers use a combination of old, ineffective and time-consuming tools, leaving them with a patchwork communication system. Inevitably, this patchwork is inefficient and insufficient, forcing staff to resort to an unreasonable amount of meetings and conversations, exchanging details that should have been shared with a click of a button.
But what is the solution?
The temptation to fall back to old habits or squeeze a functionality in existing software is usually overwhelming, so even though the solution is straight-forward, it is anything but obvious.
Healthcare communication platforms (HCPs). These are integrated solutions that are designed to enable communication between healthcare workers, including office, field and at-home staff, as well as with partners outside the own organization, including clients and their families.

HCPs have experienced a surge in popularity for good reason. Not only can they help improve communication amongst healthcare teams, but they can also lead to time and cost savings, better collaboration between departments, and better patient care. Other benefits that are frequently reported include: improved communication and streamlined workflows, reduction of phone tag, decreased consultation time and a more collaborative work environment to improve the level of care provided to patients.
It is important to note that HCPs are not meant to replace EHRs, but to enhance it. They bridge the gap in communication by connecting key staff, making patient data actionable, and effectively merging data into a single solution.
Even though the range of functionalities differ, HCPs are meant to not only improve care collaboration but also to engage patients. They provide secure, HIPAA-compliant communication for healthcare providers that need fast response times and seamless care coordination. By enabling quick and protected exchange of information between all members of a patient’s care team, including the patient themselves, secure HCPs, that usually include an enterprise messaging application out of the box, enable high-quality and efficient care. In particular, when a patient relies on home care, HCPs provide a quick, secure and compliant way for the home-based care team to coordinate with doctors, therapists, health care staff in the hospital and pharmacies, as well as the patient and patient’s family.
When choosing your HCP, there are a few key things to look out for:
What it comes down to is finding solutions with which we can improve our homecare system and improve care for our patients. The fastest and easiest way to do this is to have meaningful adoption of connected communication systems to drive improvements in cost, quality and care experiences.
HCPs are the tool with which we can achieve this. Luckily, they are very low cost, especially compared to the obvious benefits they bring, can be implemented quickly, and deliver results from day one. With a viable alternative at your fingertips, the time of inefficient and insecure patchwork communication in care is finally over.
Schedule a demo today to find more about nooa.
To have a successful team, communication is key. Here's how to communicate more effectively.
Everyone is involved in at least one of these during their career - whether as a manager, project leader or user. You guessed it: IT projects.
Structure improves working conditions, reduces stress, and increases productivity. For your benefit: we also have 6 practical tips for keeping things...
Subscribe to our magazine and be the first to know about new insights in home care.